New Therapeutic Angiogenesis Biomarkers for Chronic Diabetic Foot Ulcers Treated with Transdermal Hyperoxia/Topical Wound Oxygen (TWO2)
Gary F. Scott, Ph.D.
Department of Cell Biology and Genetics, University of North Texas Health Science Center, Fort Worth, Texas 76107
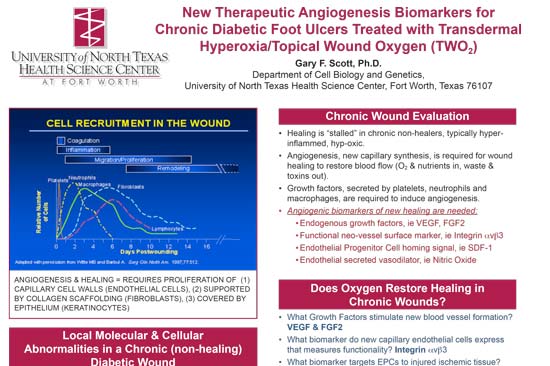
ANGIOGENESIS & HEALING = REQUIRES PROLIFERATION OF (1) CAPILLARY CELL WALLS (ENDOTHELIAL CELLS), (2) SUPPORTED BY COLLAGEN SCAFFOLDING (FIBROBLASTS), (3) COVERED BY EPITHELIUM (KERATINOCYTES)
Local Molecular & Cellular Abnormalities in a Chronic (non-healing) Diabetic Wound
• Growth factor and cytokine deficiencies • Endothelial dysfunction • Neuropathy: associated with endothelium dependent and independent dysfunction in diabetics predisposed to foot ulceration • Arterial occlusive disease (PAD): associated with peripheral neuropathy, slower conduction velocity of sensory nerves, depression of autonomic responses • Abnormalities in fibroblast function • Abnormalities in extracellular matrix and decreased cellular infiltrate • Decreased angiogenesis (thus sustained O2 deprivation)
Oxygen in Tissues and Wounds
• All nucleated cells use O2 energy metabolism (via mitochondria) • Epidermis into papillary dermis use transdermal O2 • From blood Hb, O2 diffusion through membranes into is “concentration” dependent In wounds, vessels disrupted, so lack O2 • Wound ischemic hypoxia impairs O2-ase enzymes • Cytochrome O2-ase for ATP generation, uses 8O% of O2 breathed • Prolyl hydroxylase for collagen synthesis, req. for angiogenesis • Phagocytic O2-ase for bacteria killing via ‘respiratory burst’ Obvious rationale for supplemental O2 Enforced O2 concentration (TWO2) increases diffusion distance Renewed O2 supply can activate repair molecules Highest priority to restore O2, thus angiogenesis required!!
Chronic Wound Evaluation
• Healing is “stalled” in chronic non-healers, typically hyperinflammed, hyp-oxic. • Angiogenesis, new capillary synthesis, is required for wound healing to restore blood flow (O2 & nutrients in, waste & toxins out). • Growth factors, secreted by platelets, neutrophils and macrophages, are required to induce angiogenesis. • Angiogenic biomarkers of new healing are needed: • Endogenous growth factors, ie VEGF, FGF2 • Functional neo-vessel surface marker, ie Integrin avb3 • Endothelial Progenitor Cell homing signal, ie SDF-1 • Endothelial secreted vasodilator, ie Nitric Oxide
Does Oxygen Restore Healing in Chronic Wounds?
• What Growth Factors stimulate new blood vessel formation? VEGF & FGF2 • What biomarker do new capillary endothelial cells express that measures functionality? Integrin avb3 • What biomarker targets EPCs to injured ischemic tissue? SDF-1 • What O2-sensitive molecules deficient in chronic wounds respond to TWO2? VEGF, FGF2, Integrin avb3, SDF-1
Treatments and Wound Fluid Collection
• Topical Wound Oxygen Treatments (TWO2) were administered with medical grade oxygen (>95% pure) in a TOCE (Topical Oxygen Chamber for Extremities) for 4 consecutive days, 90 minutes per treatment for 5 weeks. • Wounds were digitally photographed and wound fluids were collected after treatment on day one and day four of each week’s treatments. • Fluids from the wound bed were absorbed onto a cotton swab by wiping to collect maximum fluid exudates’ volume. Trimmed swabs containing wound fluids were solubilized in 0.1 M Phosphate Buffered Solution (PBS), fractionated by centrifugation and stored at –20oC for subsequent assay • Simultaneous quantification of analytes was performed using a customized multiplex enzyme-linked immunosorbent assay (ELISA) at end of 5 weeks of treatment. Total protein in samples was measured. • Analyte concentration changes per unit of total protein standardized for sample volume variance. • In current ongoing studies, baseline wound fluid samples are collected weekly for 2 weeks prior to treatment for treatment effect comparison.
Summary of Results of Therapeutic Angiogenic BioMarkers During Transdermal Hyperoxia (TWO2 ) Treatments
• Angiogenic Growth Factors VEGF &FGF-2 increased significantly • Integrin aVb3 (only transiently expressed in new endothelial membrane) increases correspond to angiogenic growth factors’ changes • confirms formation of new functional capillaries and O2 re-supply • not previously quantified in human wound fluids • SDF-1 targets BMEPCs (bone marrow-derived endothelial progenitor cells) to injury site (vasculogenesis augments angiogenesis)
Conclusions
- This physiologically relevant set of biomarkers quantify therapeutic
angiogenesis indicating evidence of renewed activation of dormant cells in chronic wounds, and thus healing.
- These ‘endogenous’ angiogenic biomarkers as surrogate end-points of healing provide evidence allowing comparison of treatment benefits at far earlier timepoints than ultimate clinical endpoints, i.e. full wound
- This mechanism of action analysis of wound responses to transdermal hyperoxia treatment (TWO2) demonstrates efficacy that reduces costs while improving benefits to a larger number of patients.
References
- Diabetic cellular dysfunctions Lerman OZ, Galiano RG, Armour M, Levine JP, Gurtner GP. Cellular dysfunction in the diabetic fibroblast: impairment in migration, vascular endothelial growth factor production, and response to hypoxia. Am J Pathol. 2003;162:303-312.
- VEGF/FGF2 Kano MR et al. VEGF-A and FGF-2 synergistically promote neoangiogenesis through enhancement of endogenous PDGF-B-PDGFRbeta signaling. J Cell Sci. 2005;118:3759-3768. Stavri GT et al. Basic fibroblast growth factor up-regulates the expression of vascular endothelial growth factor in vascular smooth muscle: Synergistic interaction with hypoxia. Circulation. 1995;92:11-14.
- Integrin avb3 Clark RA, Tonnesen MG, Gailit J, Cheresh DA. Transient functional expression of avb3 on vascular cells during wound repair. Am J Pathol. 1996;148:1407-1421.
- SDF-1 Gallagher, K.A., et al. 2007. Diabetic impairments in NO-mediated endothelial progenitor cell mobilization and homing are reversed by hyperoxia and SDF-1α. J. Clin. Invest. 117:1249-1259