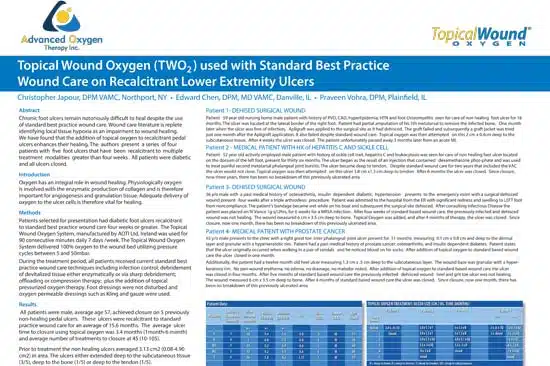
Topical Wound Oxygen (TWO2) used with Standard Best Practice Wound Care on Recalcitrant Lower Extremity Ulcers
Christopher Japour, DPM VAMC, Northport, NY • Edward Chen, DPM, MD VAMC, Danville, IL • Praveen Vohra, DPM, Plainfield, IL
Abstract
Chronic foot ulcers remain notoriously difficult to heal despite the use of standard best practice wound care. Wound care literature is replete
identifying local tissue hypoxia as an impairment to wound healing. We have found that the addition of topical oxygen to recalcitrant pedal
ulcers enhances their healing. The authors present a series of four patients with five foot ulcers that have been recalcitrant to multiple
treatment modalities greater than four weeks. All patients were diabetic and all ulcers closed.
Introduction
Oxygen has an integral role in wound healing. Physiologically oxygen is involved with the enzymatic production of collagen and is therefore
important for angiogenesis and granulation tissue. Adequate delivery of oxygen to the ulcer cells is therefore vital for healing.
Methods
Patients selected for presentation had diabetic foot ulcers recalcitrant to standard best practice wound care four weeks or greater. The Topical Wound Oxygen System, manufactured by AOTI Ltd, Ireland was used for 90 consecutive minutes daily 7 days /week. The Topical Wound Oxygen System delivered 100% oxygen to the wound bed utilizing pressure cycles between 5 and 50mbar.
During the treatment period, all patients received current standard best practice wound care techniques including infection control; debridement
of devitalized tissue either enzymatically or via sharp debridement; offloading or compression therapy; plus the addition of topical
pressurized oxygen therapy. Foot dressings were not disturbed and oxygen permeable dressings such as Kling and gauze were used.
Results
All patients were male, average age 57, achieved closure on 5 previously non-healing pedal ulcers. These ulcers were recalcitrant to standard
practice wound care for an average of 15.6 months. The average ulcer time to closure using topical oxygen was 3.4 months (1 month-6 month)
and average number of treatments to closure at 45 (10-105). Prior to treatment the non healing ulcers averaged 3.13 cm2 (0.08-4.90
cm2) in area. The ulcers either extended deep to the subcutaneous tissue (3/5), deep to the bone (1/5) or deep to the tendon (1/5).
Patient 1-DEHISED SURGICAL WOUND
Patient 59 year old nursing home male patient with history of PVD, CAD, hyperlipidemia, HTN and foot Osteomyelitis seen for care of non healing foot ulcer for 18 months. The ulcer was located at the lateral border of the right foot. Patient had partial amputation of his 5th metatarsal to remove the infected bone. One month later when the ulcer was free of infection, Apligraft was applied to the surgical site as it had dehisced. The graft failed and subsequently a graft jacket was tried just one month after the Apligraft application. It also failed despite standard wound care. Topical oxygen was then attempted on this 2 cm x 0.4cm deep to the subcutaneous tissue. After 4 weeks the ulcer was closed. The patient unfortunately passed away 3 months later from an acute Ml.
Patient 2- MEDICAL PATIENT WITH HX of HEPATITICS AND SICKLE CELL
Patient 52 year old actively employed male patient with history of sickle cell trait, hepatitis C and leukocytosis was seen for care of non healing foot ulcer located on the dorsum of the left foot, present for thirty six months. The ulcer began as the result of an injection that contained dexamethasone phos-phate and was used to treat painful second metatarsal phalangeal joint bursitis. The ulcer became deep to tendon. Despite standard wound care for two years that included the VAC the ulcer would not close. Topical oxygen was then attempted on this ulcer 3.8 cm x1 .3 cm deep to tendon. After 6 months the ulcer was closed. Since closure, now three years, there has been no breakdown of this previously ulcerated area.
Patient 3- DEHISED SURGICAL WOUND
56 y/o male with a past medical history of osteoarthritis, insulin dependent diabetic, hypertension presents to the emergency room with a surgical dehisced wound present four weeks after a triple arthrodesis procedure. Patient was admitted to the hospital from the ER with significant redness and swelling to LEFT foot from noncompliance. The patient’s bandage became wet while on his boat and subsequent the surgical site dehisced. After consulting Infectious Disease the patient was placed on IVVanco 1gq12hrs, for 6 weeks for a MRSA infection. After four weeks of standard based wound care, the previously infected and dehisced wound was not healing. The wound measured 6 cm x 3.5 cm deep to bone. Topical Oxygen was added, and after4 months of therapy, the ulcer was closed. Since closure, now one month, there has been no breakdown of this previously ulcerated area.
Patient 4- MEDICAL PATIENT WITH PROSTATE CANCER
65 y/o male presents to the clinic with a right great toe inter phalangeal joint ulcer present for 11 months measuring 0.1 cm x 0.8 cm and deep to the dermal layer and granular with a hyperkeratotic rim. Patient had a past medical history of prostate cancer, osteoarthritis, and insulin dependent diabetes. Patient states that the ulcer originally occurred when walking in a pair of sandals and he noticed blood on his socks. After addition of topical oxygen to standard based wound care the ulcer closed in one month. Additionally, the patient had a twelve month old heel ulcer measuring 1.3 cm x .5 cm deep to the subcutaneous layer. The wound base was granular with a hyperkeratosis rim. No peri-wound erythema, no edema, no drainage, no malodor noted. After addition of topical oxygen to standard based wound care the ulcer was closed in four months. After five months of standard based wound care the previously infected dehisced wound heel and grit toe ulcer was not healing. The wound measured 6 cm x 3.5 cm deep to bone. After 4 months of standard based wound care the ulcer was closed. Since closure, now one month, there has been no breakdown of this previously ulcerated area.