Multi-Modality Approach to Healing a Diabetic Neuroischemic Partial Thickness Burn: The Use of Topical Wound Oxygen with Human Amniotic Membrane
Aliza Lee, DPM, MS, PGY-3; Paul Shearer, DPM Veterans Affairs Medical Center-Salem, VA
Purpose
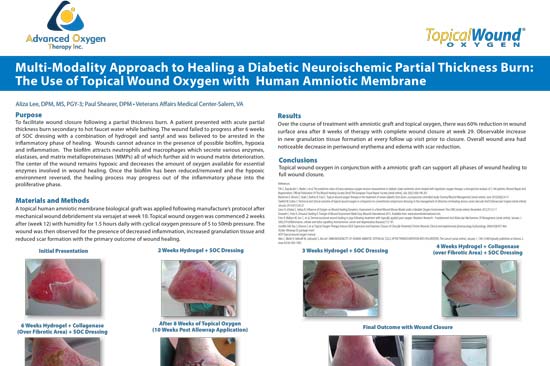
To facilitate wound closure following a partial thickness burn. A patient presented with acute partial thickness burn secondary to hot faucet water while bathing. The wound failed to progress after 6 weeks of SOC dressing with a combination of hydrogel and santyl and was believed to be arrested in the inflammatory phase of healing. Wounds cannot advance in the presence of possible biofilm, hypoxia and inflammation. The biofilm attracts neutrophils and macrophages which secrete various enzymes, elastases, and matrix metalloproteinases (MMPs) all of which further aid in wound matrix deterioration. The center of the wound remains hypoxic and decreases the amount of oxygen available for essential enzymes involved in wound healing. Once the biofilm has been reduced/removed and the hypoxic environment reversed, the healing process may progress out of the inflammatory phase into the proliferative phase.
Materials and Methods
A topical human amniotic membrane biological graft was applied following manufacture’s protocol after mechanical wound debridement via versajet at week 10. Topical wound oxygen was commenced 2 weeks after (week 12) with humidity for 1.5 hours daily with cyclical oxygen pressure of 5 to 50mb pressure. The wound was then observed for the presence of decreased inflammation, increased granulation tissue and reduced scar formation with the primary outcome of wound healing.
Results
Over the course of treatment with amniotic graft and topical oxygen, there was 60% reduction in wound surface area after 8 weeks of therapy with complete wound closure at week 29. Observable increase in new granulation tissue formation at every follow up visit prior to closure. Overall wound area had noticeable decrease in periwound erythema and edema with scar reduction.
Conclusions
Topical wound oxygen in conjunction with a amniotic graft can support all phases of wound healing to full wound closure.
References:
Fife C, Buyukcakir C, Mader J, et al. The predictive value of transcutaneous oxygen tension measurement in diabetic lower extremity ulcers treated with hyperbaric oxygen therapy: a retrospective analysis of 1,144 patients. Wound Repair And Regeneration: Official Publication Of The Wound Healing Society [And] The European Tissue Repair Society [serial online]. July 2002;10(4):198-207.
Blackman E, Moore C, Hyatt J, Railton R, Frye C. Topical wound oxygen therapy in the treatment of severe diabetic foot ulcers: a prospective controlled study. Ostomy/Wound Management [serial online]. June 2010;56(6):24-31.
Tawfick W, Sultan S. Technical and clinical outcome of topical wound oxygen in comparison to conventional compression dressings in the management of refractory nonhealing venous ulcers. Vascular And Endovascular Surgery [serial online]. January 2013;47(1):30-37.
Sano H, Ichioka S, Sekiya N. Influence of Oxygen on Wound Healing Dynamics: Assessment in a Novel Wound Mouse Model under a Variable Oxygen Environment. Plos ONE [serial online]. November 2012;7(11):1-7. Dowsett C, Protz K, Drouard, Harding K. Triangle of Wound Assessment Made Easy. Wounds International 2015. Available from: www.woundsinternational.com.
Fries R, Wallace W, Sen C, et al. Dermal excisional wound healing in pigs following treatment with topically applied pure oxygen. Mutation Research – Fundamental And Molecular Mechanisms Of Mutagenesis [serial online]. January 1, 2005;579 (Inflammation, cellular and redox signalling mechanismsin cancer and degenerative diseases):172-181.
Gordillo GM, Roy S, Khanna S, et al. Topical Oxygen Therapy Induces VEGF Expression and Improves Closure of Clinically Presented Chronic Wounds. Clinical and experimental pharmacology & physiology. 2008;35(8):957-964. Stryker Allowrap DS package insert
AOTi Topical wound oxygen manual
Akle C, Welsh K, Adinolfi M, Leibowitz S, Mccoll I. IMMUNOGENICITY OF HUMAN AMNIOTIC EPITHELIAL CELLS AFTER TRANSPLANTATION INTO VOLUNTEERS. The Lancet [serial online]. January 1, 1981;318(Originally published as Volume 2, Issue 8254):1003-1005.