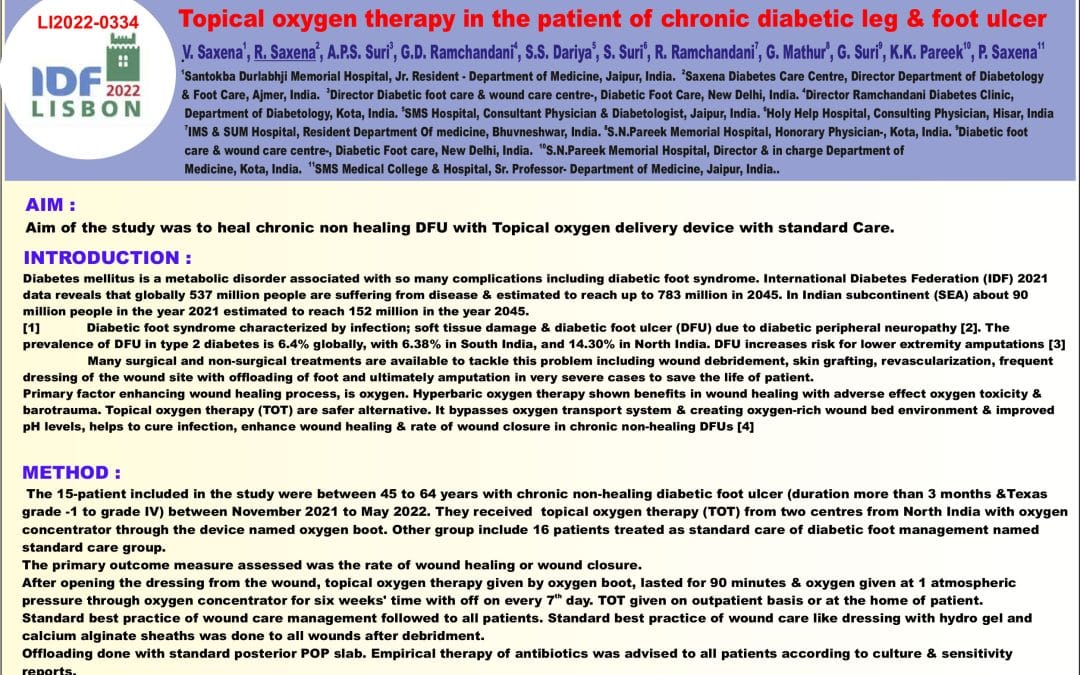
Topical oxygen therapy in the patient of chronic diabetic leg & foot ulcer
V. Saxena, R. Saxena, A.P.S. Suri, G.D. Ramchandani, S.S. Dariya, S. Suri, R. Ramchandani, G. Mathur, G. Suri, K.K. Pareek, P. Saxena
Topical oxygen therapy in the patient of chronic diabetic leg & foot ulcer . 1 2 Santokba Durlabhji Memorial Hospital, Jr. Resident – Department of Medicine, Jaipur, India. Saxena Diabetes Care Centre, Director Department of Diabetology 3 4 & Foot Care, Ajmer, India. Director Diabetic foot care & wound care centre-, Diabetic Foot Care, New Delhi, India. Director Ramchandani Diabetes Clinic, 5 6 Department of Diabetology, Kota, India. SMS Hospital, Consultant Physician & Diabetologist, Jaipur, India. Holy Help Hospital, Consulting Physician, Hisar, India 7 8 9 IMS & SUM Hospital, Resident Department Of medicine, Bhuvneshwar, India. S.N.Pareek Memorial Hospital, Honorary Physician-, Kota, India. Diabetic foot 10 care & wound care centre-, Diabetic Foot care, New Delhi, India. S.N.Pareek Memorial Hospital, Director & in charge Department of 11 Medicine, Kota, India. SMS Medical College & Hospital, Sr. Professor- Department of Medicine, Jaipur, India..
AIM :
Aim of the study was to heal chronic non healing DFU with Topical oxygen delivery device with standard Care.
INTRODUCTION :
Diabetes mellitus is a metabolic disorder associated with so many complications including diabetic foot syndrome. International Diabetes Federation (IDF) 2021 data reveals that globally 537 million people are suffering from disease & estimated to reach up to 783 million in 2045. In Indian subcontinent (SEA) about 90 million people in the year 2021 estimated to reach 152 million in the year 2045. [1] Diabetic foot syndrome characterized by infection; soft tissue damage & diabetic foot ulcer (DFU) due to diabetic peripheral neuropathy [2]. The prevalence of DFU in type 2 diabetes is 6.4% globally, with 6.38% in South India, and 14.30% in North India. DFU increases risk for lower extremity amputations [3] Many surgical and non-surgical treatments are available to tackle this problem including wound debridement, skin grafting, revascularization, frequent dressing of the wound site with offloading of foot and ultimately amputation in very severe cases to save the life of patient. Primary factor enhancing wound healing process, is oxygen. Hyperbaric oxygen therapy shown benefits in wound healing with adverse effect oxygen toxicity & barotrauma. Topical oxygen therapy (TOT) are safer alternative. It bypasses oxygen transport system & creating oxygen-rich wound bed environment & improved pH levels, helps to cure infection, enhance wound healing & rate of wound closure in chronic non-healing DFUs [4]
METHOD :
The 15-patient included in the study were between 45 to 64 years with chronic non-healing diabetic foot ulcer (duration more than 3 months &Texas grade -1 to grade IV) between November 2021 to May 2022. They received topical oxygen therapy (TOT) from two centres from North India with oxygen concentrator through the device named oxygen boot. Other group include 16 patients treated as standard care of diabetic foot management named standard care group. The primary outcome measure assessed was the rate of wound healing or wound closure. After opening the dressing from the wound, topical oxygen therapy given by oxygen boot, lasted for 90 minutes & oxygen given at 1 atmospheric th pressure through oxygen concentrator for six weeks’ time with off on every 7 day. TOT given on outpatient basis or at the home of patient. Standard best practice of wound care management followed to all patients. Standard best practice of wound care like dressing with hydro gel and calcium alginate sheaths was done to all wounds after debridment. Offloading done with standard posterior POP slab. Empirical therapy of antibiotics was advised to all patients according to culture & sensitivity reports.- All wounds included in study were Texas grade -1 to grade IV st th-In each patient’s follow-up of culture & sensitivity done on day 1, 7& 21.-Blood perfusion was normal in all patient, ABI was normal i.e.between 0.8-1.2-Neurological assessment by VPT, severe diabetic peripheral neuropathy presents i.e., VPT threshold between 42 to 45-Creatinine was between 1.2 to 2.6 mg%.-All patient on anti-platelets therapy advised Rivaroxaban 2.5 mg + aspirin 75 mg-All patients on OHA with basal insulin or Mixtared. Data were prospectively obtained on wound size, duration of Ulcer, glycaemic control, neuropathy assessment by vibration perception test (VPT), vascular assessment by ABI & colour Doppler, renal function etc.
RESULTS :
In TOT group Wound granulated in 4 weeks and reduction in bio film by 1weak.Smell of wound reduced after 4-5 sitting with size of wound reduced by more than 50 % of surface area by 4 to 6 weeks & complete healing of wound in 60 % of patient in the study time frame within 8 to 10 weeks. 4 patient in 10 to 12 weeks & 2 patients require skin grafting after coming of granulation. Healing time is about 2 to 4 weeks early then standard group.
CONCLUSIONS :
The application of topical oxygen therapy (TOT) in patients with Texas grade I to 4 of chronic diabetic foot ulcers improves wound healing.In Grade 1 & 2 complete healing of ulcer & in higher grade reduction of size up[to 50 to 80 % along with depth of ulcer in study time frame i.e. 8 to 10 weeks. The topical oxygen therapy represents a potentially exciting new technology to decrease healing time and to promote wound closure in patients with nonhealing DFUs. More studies are needed to determine the benefits of topical oxygen, but our current results are extremely promising. Conflict of Interest: I have no potential conflict of interest to disclose.
CONFLICT OF INTEREST: NO CONFLICT OF INTEREST
References: 1. IDF diabetes atlas – 10 edition 2021.Across the globe http://www.diabetesatlas.org/across-the-globe.html. 2.Jakosz N. IWGDF guidelines on the prevention and management of diabetic foot disease (book review). Wound practice and research. Wound Repair Regen. 2019; 27(3):144. [Google Scholar 3.Shahi SK, Kumar A, Kumar S, Singh SK, Gupta SK, Singh TB. Prevalence of diabetic foot ulcer and associated risk factors in diabetic patients from North India. J Diabet Foot Compl. 2012;4(3):83–91. [Google Scholar] 4.Demling RH. Nutrition, anabolism, and the wound healing process: anverview. Eplasty. 2009;9:e9. [PMC free article] [PubMed] [Google Scholar