Adjunct Intermittent Topical Oxygen Therapy Promotes Closure in Calciphylaxis Wounds Laurin Mejia, Ph.D., PA-C, CWS1 , Karin Zachow, MD, CWS 1 1 Bruce W Carter VA Medical Center, Miami, FL.
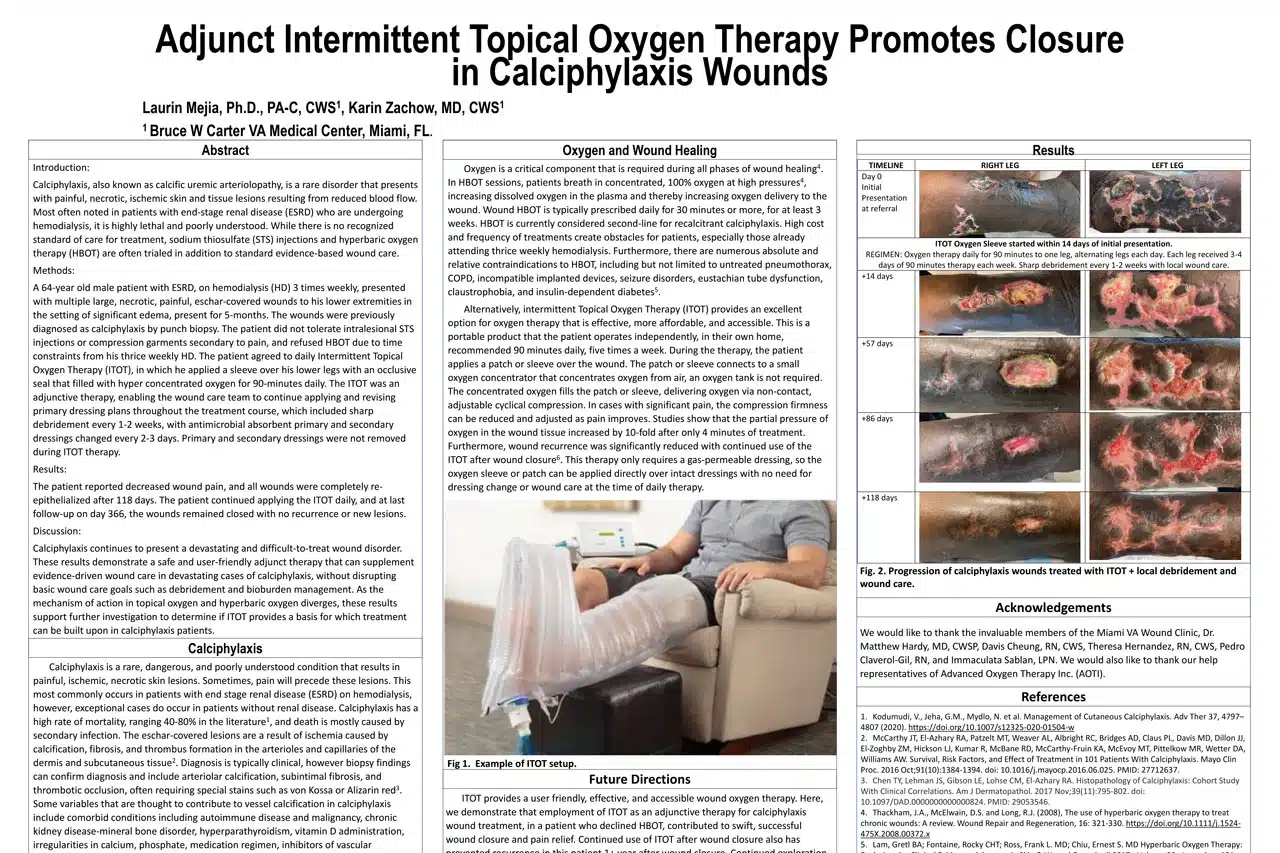
Introduction: Calciphylaxis, also known as calcific uremic arteriolopathy, is a rare disorder that presents with painful, necrotic, ischemic skin and tissue lesions resulting from reduced blood flow. Most often noted in patients with end-stage renal disease (ESRD) who are undergoing hemodialysis, it is highly lethal and poorly understood. While there is no recognized standard of care for treatment, sodium thiosulfate (STS) injections and hyperbaric oxygen therapy (HBOT) are often trialed in addition to standard evidence-based wound care. Methods: A 64-year old male patient with ESRD, on hemodialysis (HD) 3 times weekly, presented with multiple large, necrotic, painful, eschar-covered wounds to his lower extremities in the setting of significant edema, present for 5-months. The wounds were previously diagnosed as calciphylaxis by punch biopsy. The patient did not tolerate intralesional STS injections or compression garments secondary to pain, and refused HBOT due to time constraints from his thrice weekly HD. The patient agreed to daily Intermittent Topical Oxygen Therapy (ITOT), in which he applied a sleeve over his lower legs with an occlusive seal that filled with hyper concentrated oxygen for 90-minutes daily. The ITOT was an adjunctive therapy, enabling the wound care team to continue applying and revising primary dressing plans throughout the treatment course, which included sharp debridement every 1-2 weeks, with antimicrobial absorbent primary and secondary dressings changed every 2-3 days. Primary and secondary dressings were not removed during ITOT therapy. Results: The patient reported decreased wound pain, and all wounds were completely reepithelialized after 118 days. The patient continued applying the ITOT daily, and at last follow-up on day 366, the wounds remained closed with no recurrence or new lesions. Discussion: Calciphylaxis continues to present a devastating and difficult-to-treat wound disorder. These results demonstrate a safe and user-friendly adjunct therapy that can supplement evidence-driven wound care in devastating cases of calciphylaxis, without disrupting basic wound care goals such as debridement and bioburden management. As the mechanism of action in topical oxygen and hyperbaric oxygen diverges, these results support further investigation to determine if ITOT provides a basis for which treatment can be built upon in calciphylaxis patients.
Calciphylaxis
Calciphylaxis is a rare, dangerous, and poorly understood condition that results in painful, ischemic, necrotic skin lesions. Sometimes, pain will precede these lesions. This most commonly occurs in patients with end stage renal disease (ESRD) on hemodialysis, however, exceptional cases do occur in patients without renal disease. Calciphylaxis has a high rate of mortality, ranging 40-80% in the literature1 , and death is mostly caused by secondary infection. The eschar-covered lesions are a result of ischemia caused by calcification, fibrosis, and thrombus formation in the arterioles and capillaries of the dermis and subcutaneous tissue2 . Diagnosis is typically clinical, however biopsy findings can confirm diagnosis and include arteriolar calcification, subintimal fibrosis, and thrombotic occlusion, often requiring special stains such as von Kossa or Alizarin red3 . Some variables that are thought to contribute to vessel calcification in calciphylaxis include comorbid conditions including autoimmune disease and malignancy, chronic kidney disease-mineral bone disorder, hyperparathyroidism, vitamin D administration, irregularities in calcium, phosphate, medication regimen, inhibitors of vascular calcification, and chronic inflammation. Treatments targeting these features will sometimes benefit patients, however there are still no definitive guidelines for calciphylaxis treatment. Typically, the initial approach includes pain control, wound care, and managing risk factors. Other common components of treatment include sodium thiosulfate, parathyroidectomy, surgical debridement, and hyperbaric oxygen therapy (HBOT).
Oxygen and Wound Healing
Oxygen is a critical component that is required during all phases of wound healing 4 . In HBOT sessions, patients breath in concentrated, 100% oxygen at high pressures 4 , increasing dissolved oxygen in the plasma and thereby increasing oxygen delivery to the wound. Wound HBOT is typically prescribed daily for 30 minutes or more, for at least 3 weeks. HBOT is currently considered second-line for recalcitrant calciphylaxis. High cost and frequency of treatments create obstacles for patients, especially those already attending thrice weekly hemodialysis. Furthermore, there are numerous absolute and relative contraindications to HBOT, including but not limited to untreated pneumothorax, COPD, incompatible implanted devices, seizure disorders, eustachian tube dysfunction, claustrophobia, and insulin-dependent diabetes 5 . Alternatively, intermittent Topical Oxygen Therapy (ITOT) provides an excellent option for oxygen therapy that is effective, more affordable, and accessible. This is a portable product that the patient operates independently, in their own home, recommended 90 minutes daily, five times a week. During the therapy, the patient applies a patch or sleeve over the wound. The patch or sleeve connects to a small oxygen concentrator that concentrates oxygen from air, an oxygen tank is not required. The concentrated oxygen fills the patch or sleeve, delivering oxygen via non-contact, adjustable cyclical compression. In cases with significant pain, the compression firmness can be reduced and adjusted as pain improves. Studies show that the partial pressure of oxygen in the wound tissue increased by 10-fold after only 4 minutes of treatment. Furthermore, wound recurrence was significantly reduced with continued use of the ITOT after wound closure 6 . This therapy only requires a gas-permeable dressing, so the oxygen sleeve or patch can be applied directly over intact dressings with no need for dressing change or wound care at the time of daily therapy.
Future Directions
ITOT provides a user friendly, effective, and accessible wound oxygen therapy. Here, we demonstrate that employment of ITOT as an adjunctive therapy for calciphylaxis wound treatment, in a patient who declined HBOT, contributed to swift, successful wound closure and pain relief. Continued use of ITOT after wound closure also has prevented recurrence in this patient 1+ year after wound closure. Continued exploration of ITOT in additional cases of calciphylaxis and non-uremic calciphylaxis, as well as other ischemic wound etiologies is warranted. Furthermore, as the mechanisms of ITOT is independent of oxygen intake in the lungs, it would provide valuable information to explore the efficacy of ITOT vs HBOT for wound therapy in patients with gas-exchange diseases such as COPD or asthma, which are relative contraindications in HBOT
Acknowledgements
We would like to thank the invaluable members of the Miami VA Wound Clinic, Dr. Matthew Hardy, MD, CWSP, Davis Cheung, RN, CWS, Theresa Hernandez, RN, CWS, Pedro Claverol-Gil, RN, and Immaculata Sablan, LPN. We would also like to thank our help representatives of Advanced Oxygen Therapy Inc. (AOTI).
References
1. Kodumudi, V., Jeha, G.M., Mydlo, N. et al. Management of Cutaneous Calciphylaxis. Adv Ther 37, 4797– 4807 (2020). https://doi.org/10.1007/s12325-020-01504-w 2. McCarthy JT, El-Azhary RA, Patzelt MT, Weaver AL, Albright RC, Bridges AD, Claus PL, Davis MD, Dillon JJ, El-Zoghby ZM, Hickson LJ, Kumar R, McBane RD, McCarthy-Fruin KA, McEvoy MT, Pittelkow MR, Wetter DA, Williams AW. Survival, Risk Factors, and Effect of Treatment in 101 Patients With Calciphylaxis. Mayo Clin Proc. 2016 Oct;91(10):1384-1394. doi: 10.1016/j.mayocp.2016.06.025. PMID: 27712637. 3. Chen TY, Lehman JS, Gibson LE, Lohse CM, El-Azhary RA. Histopathology of Calciphylaxis: Cohort Study With Clinical Correlations. Am J Dermatopathol. 2017 Nov;39(11):795-802. doi: 10.1097/DAD.0000000000000824. PMID: 29053546. 4. Thackham, J.A., McElwain, D.S. and Long, R.J. (2008), The use of hyperbaric oxygen therapy to treat chronic wounds: A review. Wound Repair and Regeneration, 16: 321-330. https://doi.org/10.1111/j.1524- 475X.2008.00372.x 5. Lam, Gretl BA; Fontaine, Rocky CHT; Ross, Frank L. MD; Chiu, Ernest S. MD Hyperbaric Oxygen Therapy: Exploring the Clinical Evidence, Advances in Skin & Wound Care: April 2017 – Volume 30 – Issue 4 – p 181- 190 doi: 10.1097/01.ASW.0000513089.75457.22 6. Frykberg RG, Franks PJ, Edmonds M, Brantley JN, Téot L, Wild T, Garoufalis MG, Lee AM, Thompson JA, Reach G, Dove CR, Lachgar K, Grotemeyer D, Renton SC; TWO2 Study Group. A Multinational, Multicenter, Randomized, Double-Blinded, Placebo-Controlled Trial to Evaluate the Efficacy of Cyclical Topical Wound Oxygen (TWO2) Therapy in the Treatment of Chronic Diabetic Foot Ulcers: The TWO2 Study. Diabetes Care. 2020 Mar;43(3):616-624. doi: 10.2337/dc19-0476. Epub 2019 Oct 16. PMID: 31619393.